Update – 28 April 2021
This paper has now been published in BMC Medical Informatics and Decision Making.
Martin, C., McDonald, S., Bale, S. et al. Construction of a demand and capacity model for intensive care and hospital ward beds, and mortality from COVID-19. BMC Med Inform Decis Mak21, 138 (2021). https://doi.org/10.1186/s12911-021-01504-y
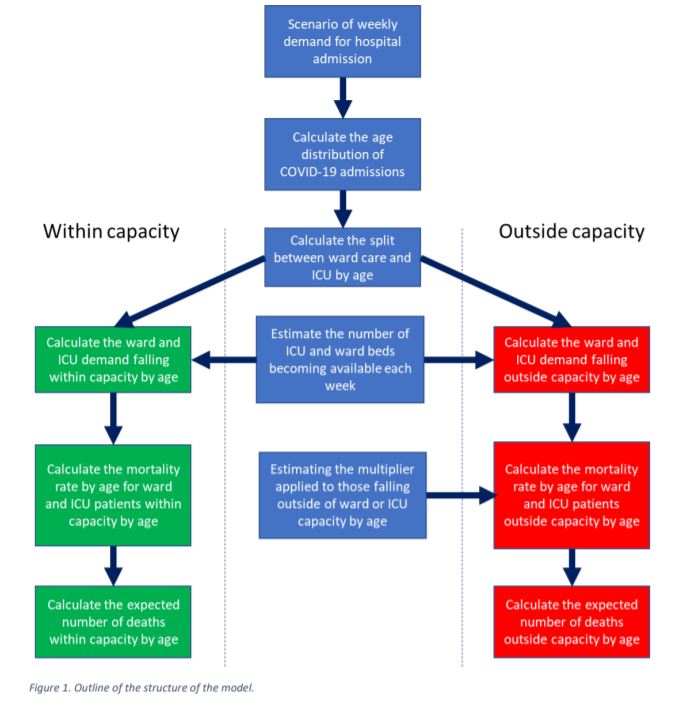
Model Framework
Yesterday a pre-print was published documenting modelling I undertook last year with a team of expert volunteers, on behalf of the Institute and Faculty of Actuaries (IFoA).
Our objective was to develop a modelling framework to examine the question of how many extra deaths arise over the 2020/21 winter period when ICU and/or general hospital capacity is exceeded.
Our model allows interested parties to look at the impact of any given scenario for hospital admissions numbers, which of course depends fundamentally on the spread of the virus. Capacity constraints are applied and can be flexed within the model to understand the impact on mortality rates.
Additional Mortality
We derived mortality scalars, following expert input from clinicians. These help us understand how much additional mortality arises when patients cannot be given the care they require.
The mortality scalars are summarised below:
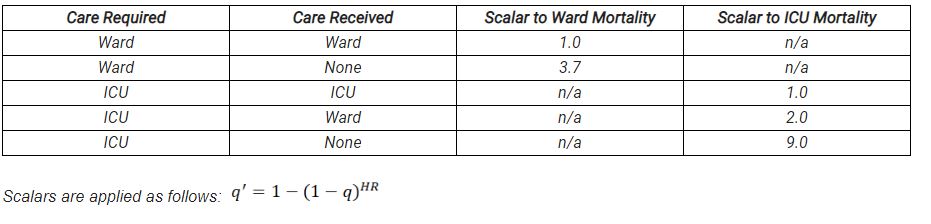
- q is the mortality rate in the required location.
- q’ is the mortality rate in the actual location.
- HR is the scalar (Hazard Ratio).
As an example, if ICU mortality at a particular age is 50% (so half survive) then the mortality of a patient who needs ICU but gets treated in the ward is 1 – (1 – 0.5)^2 = 75% (so three quarters die).
These mortality scalars are one of the key outputs of our work. Interestingly though, we found that results were much less sensitive to these scalars than to assumptions around capacity.
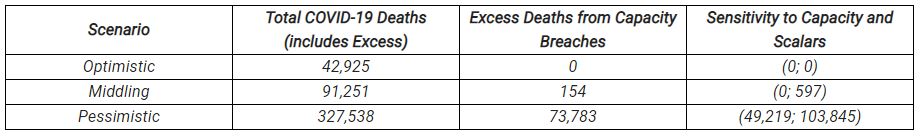
Illustrative Scenarios
To illustrate the model we produced three example scenarios for hospital admissions, which we termed “Optimistic”, “Middling” and “Pessimistic”. These scenarios are purely illustrative, they are not a key output of our modelling work and are certainly not forecasts. It is expected that users of the model, expected to be other modelling groups, will input their own scenarios.
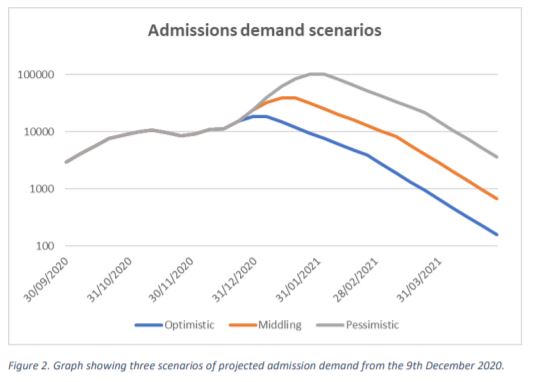
We then applied sensitivity testing to our scenarios, in particularly we flexed ICU capacity, ward capacity and the mortality scalars by 20% in each direction to understand the impacts.
Our work was completed prior to new, more transmissible, strains of the SARS-CoV-2 virus being identified. In the absence of control measures, for example the recently imposed national lockdown, these would strains significantly increase the likelihood of more pessimistic outcomes.
I am indebted to my co-authors Dr Chris Martin, Steve Bale FIA, Michiel Luteijn PhD and Dr Rahuldeb Sarkar as well as volunteers from the IFoA, Nottingham Universities Hospital Trust and Crystallise Ltd.
The pre-print paper can be found at https://www.medrxiv.org/content/10.1101/2021.01.06.21249341v1