Blog update by Nicola Oliver and Josephine Robertson
As we learn to live with the SARS-CoV-2 virus and monitor new cases our eye is on the horizon. However, with an eye in the rear view we see the wake of the pandemic i.e., the impact of infections to date in the prevalence and impact of Long COVID. Here we give an overview of what Long COVID is, what has been reported in terms of impact, prevalence, and risk factors, and an overview of the risk with regard to the QALY impact modelling and current interventions to manage the risk.
What is it?
“Long Covid” is a term used to describe illness in people who have recovered from COVID-19 but still report lasting effects of the infection, typically for longer than four weeks.
Symptoms include fatigue, chronic joint and muscle pain, insomnia, reduced exercise tolerance, shortness of breath, mental health issues including anxiety and depression, memory and concentration issues, and headaches. Clinical follow-up finds that even in mild COVID-19 infection cases, damage to the heart, lungs and brain may be permanent. A recent pre-print suggests that there may be a loss of grey matter as a result of COVID-19 which indicates potential long-term neurological sequalae [i].
Persisting symptoms seem to fall into three broad patterns:
- people who were initially hospitalised with acute respiratory distress syndrome (ARDS) and now have long-term respiratory symptoms dominated by breathlessness
- people who were not hospitalised initially but who now have a multisystem disease with evidence of cardiac, respiratory, or neurological end-organ damage manifesting in a variety of ways
- people who have persisting symptoms, often but not always dominated by fatigue, with no evidence of organ damage.
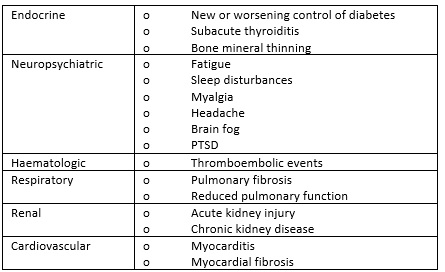
Organ damage can be categorised by system:
What has been reported?
1. Symptoms and impact to daily life
Results from the COVERSCAN study on Long Covid reports that organ impairment is detected in post COVID patients. This included damage to the heart, lungs, kidneys, liver, pancreas and spleen. In almost a third of patients, damage in two or more organs was identified. In particular, damage to the liver, heart or lungs is associated with further organ impairment. The participants in this study were all considered to be previously at low risk of mortality and had no comorbidities [ii].
The most reported symptoms are tiredness, shortness of break, muscle ache, and difficulty concentrating.
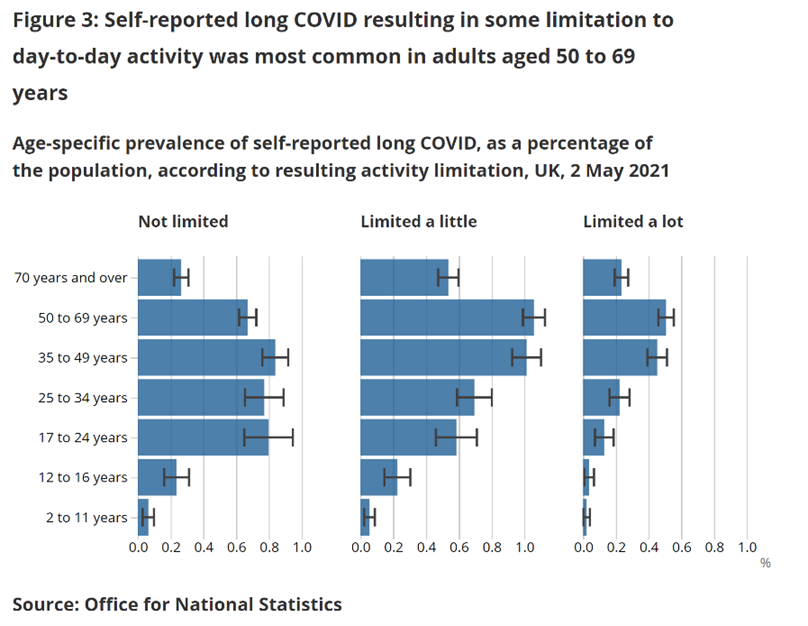
Most people with self-reported Long COVID experienced some limitation to their day-to-day activities as a result. Some report their day-to-day lives as “limited a lot” [iii]. The PHOSP-COVID study, which aims to recruit 10,000 patients who have been hospitalised with COVID-19, provides insight into the impact of UK hospitalised patient’s ability to return to work, with 19% reporting a health-related change to occupation and 18% no longer working [iv].
2. Prevalence and duration
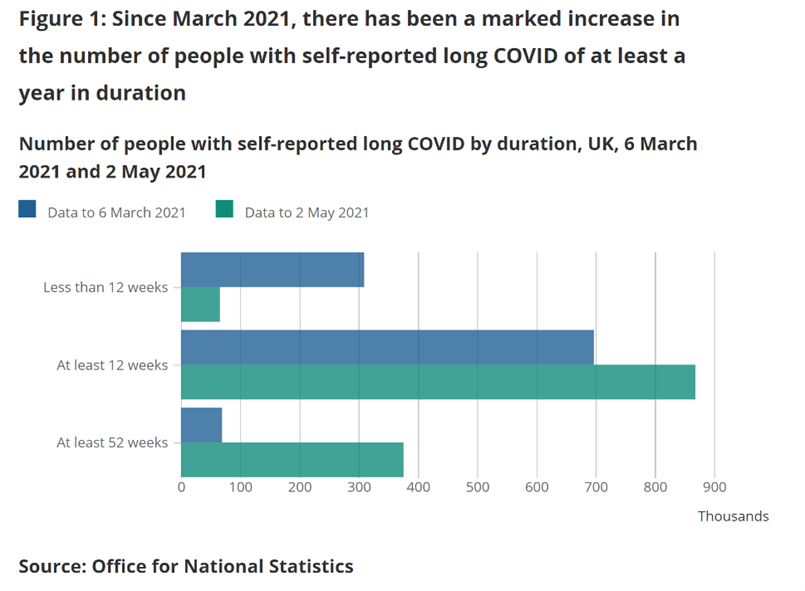
Estimates of the prevalence of self-reported Long COVID, and the duration of ongoing symptoms following confirmed coronavirus infection, using UK Coronavirus (COVID-19) Infection Survey data to 2 May 2021, suggests an estimated 1.0 million people in private households in the UK were experiencing self-reported Long COVID [v].
As data is accumulating, there appears to be an increase in the number experiencing symptoms for longer durations.
3. Who is at risk?
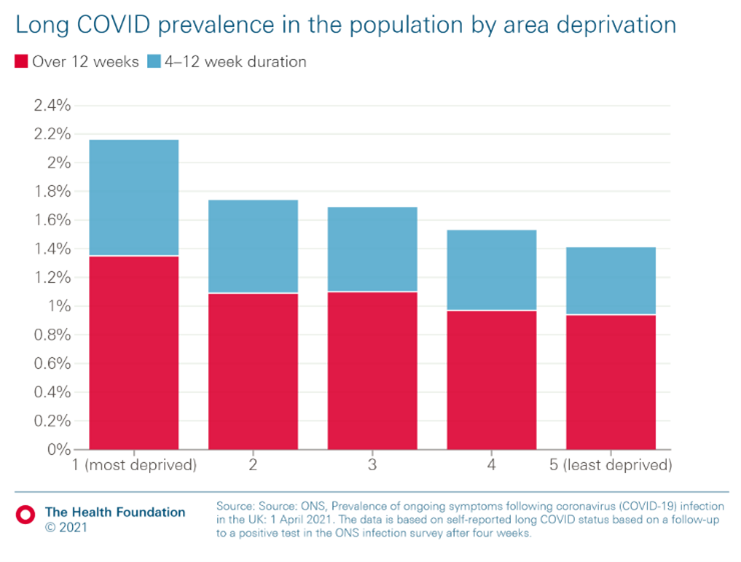
Only those who have had COVID-19 are at risk of developing Long COVID. Of those infected, the predictors of risk are not easily defined at this stage but are thought to include the presence of co-morbidities, poorer socioeconomic circumstances, hospitalisation, female sex, and potentially age, with some studies suggesting it is more prevalent in working-age groups. In one large study, (using data from the ‘Zoe’ app) the presence of five or more symptoms in the first week of illness was a strong predictor of developing Long COVID independent of age and sex.
This study found that the five symptoms experienced during the first week most predictive of long Covid were: fatigue, headache, dyspnoea, hoarse voice, and myalgia. Similar patterns were observed in men and women. In adults aged over 70, loss of smell was the most predictive of Long-COVID before fever and hoarse voice.
Prevalence rates of self-reported Long COVID are greatest for health and social care workers, and for individuals with a pre-existing, activity-limiting health condition.
Potential risks to population health and the health care system
Population health: This worrying emerging condition may represent a material future morbidity burden, with sufferers represented across age ranges and the disease severity spectrum.
Patient experience: Understanding the lived experience of Long COVID is important to build compassion in society. With a new condition, or any condition not yet well understood by the medical profession, the person suffering can be left in an unwell and under-diagnosed state. Clustered symptoms can appear in a “relapsing-remitting” nature meaning a patient can be frustratingly discharged before resolution [vi]. There is potential for “misguided assessment and treatment” by health staff and even “dismissive behaviour” from others until such time as the condition is better understood.
Health inequalities: “There is a clear social gradient in the experience of Long COVID”[vii]. Patterns by socio-demographic groups can reflect differences in infection risk and in developing Long COVID [viii]. The flexibility to accommodate lasting symptoms will vary by socio-economics status. There is scope for Long COVID to create a cascade of poor outcomes through income and employment disruption thus exacerbating health inequalities.
Staff experience: The prevalence of Long COVID is higher in the health and social care employment sector. In addition, staff in this sector have been working hard through the pandemic and at the current time have high rates of burnout [ix]. Therefore, those providing care are also in need of care at a time when a full-time complement of staff is essential.
Sustainability pressures: The NHS has been providing tertiary and preventative care for COVID-19. Beyond this are the usual health needs of the population and the added workload of overcoming the disruptions to services e.g. waiting lists [x]. Resources and capacity can be flexed but a lasting tail of increased morbidity through Long COVID may amplify existing sustainability pressures in the health and care system.
Vaccination and long COVID
Are the symptoms of Long COVID likely to be alleviated by receiving a COVID-19 vaccine? Whilst there is not yet any evidence form large scale studies, Long COVID patients are reporting alleviation of symptoms in some surveys. The advocacy group LongCovidSOS report that in the 900 people that responded to a questionnaire, 57% showed an overall reduction in their symptom score following vaccination [xi].
Professor Iwasaki from Yale University in the US has launched a new study to determine the effect of vaccination on people with persistent symptoms months after SARS-CoV-2 infection [xii].
Modelling Long COVID
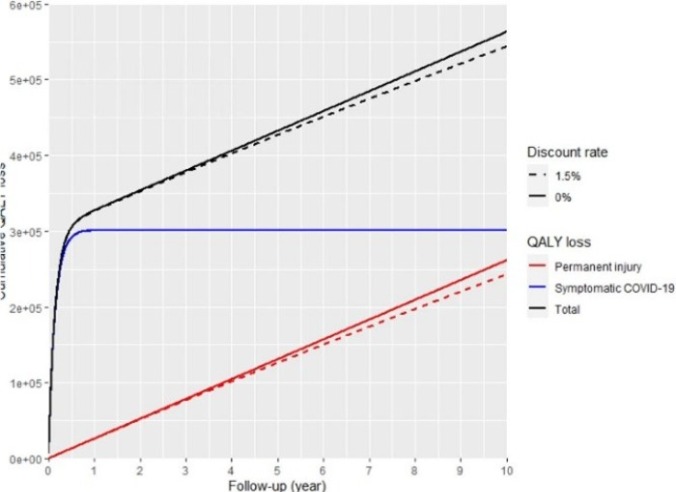
As Long COVID is new there is much about the condition which is not yet known. A group of volunteering medical researchers and actuaries have shared a model framework with “the aim of aiding the quantification and so active management of the risk of Long COVID within the UK population” [xiii].
The model framework aims to provide flexibility so the user can enter their own parameterisation and estimate a Quality Adjusted Life Years (QALYs) loss for ‘Long-COVID’. Though we are not yet in a position to parametrise this in a meaningful way.
Existing interventions to manage the risk of Long COVID
Prevention is better than cure. Aiming to prevent infections and transmission will reduce the burden of Long COVID in society. Non-pharmaceutical interventions (e.g. hands, face, space) are currently still in place and should reduce infections. Vaccinations are most effective at preventing severe disease and reduced hospitalisation may reduce the potential for Long COVID symptoms from ARDS. However, less severe infections may still present a risk of Long COVID symptoms under multisystem disease and persistent symptoms.
UK guidance published in late 2020 provides information on clinical case definition and evidence-based clinical guidelines on patient treatment [xiv]. However, the provision of online rehabilitation platforms has been critiqued as putting too much emphasis on the psychological side of Long COVID and on self-care by the patient [xv]. Designated post-COVID assessment services across England are intended to provide a multidisciplinary approach but again there is a concern that the lack of physical assessment of patients may lead to risk mismanagement and missed signs and symptoms of Long COVID. There are hypotheses that the immune response created by a COVID-19 vaccination may also reduce symptoms of Long COVID [xvi].
With the necessary research drive, information will continue to emerge on Long COVID. It is hoped that with improved understanding, improved outcomes will be possible for those with Long COVID. The WHO policy brief “In the wake of the pandemic: Preparing for Long COVID” raises awareness internationally of best practice and outlines policy options that “leave no one behind” [xvii]. Importantly this includes “[a]ction to tackle the wider consequences of Long COVID, including attention to employment rights, sick pay policies, and access to benefit and disability benefit packages”.
Summary
Ongoing reporting of the estimated prevalence and impact of Long COVID could help ensure adequate funding for research and treatment, and appropriate wider policy response. Acknowledging the lived experience of individuals with Long COVID could help ensure an empathetic response in society. This includes the importance of social cohesion in keeping cases low, even when the risk of hospitalization is reduced by vaccines, so that the health system can respond to those still in need after the initial infection.
[i] https://covidactuaries.org/wp-content/uploads/attachments/2021.06.11.21258690v1.full.pdf[ii] https://www.bmj.com/content/371/bmj.m4470 [iii] https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4june2021 [iv] https://www.medrxiv.org/content/10.1101/2021.03.22.21254057v2.full-text [v] https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4june2021 [vi] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32705-7/fulltext [vii] https://www.health.org.uk/news-and-comment/blogs/what-might-long-covid-mean-for-the-nations-health [viii] https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/4june2021 [ix] https://committees.parliament.uk/publications/6158/documents/68766/default/ [x] https://ifs.org.uk/publications/15432 [xi] https://www.pslhub.org/learn/coronavirus-covid19/data-and-statistics/the-impact-of-covid-vaccination-on-symptoms-of-long-covid-an-international-survey-of-900-people-with-lived-experience-may-2021-r4636/ [xii] https://news.yale.edu/2021/05/10/study-probes-vaccines-effects-people-long-covid[xiii] https://www.medrxiv.org/content/10.1101/2021.05.18.21252341v1[xiv] https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ [xv] https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32705-7/fulltext [xvi] https://elemental.medium.com/how-vaccines-might-improve-long-covid-c1f41c4d7378 [xvii] https://covidactuaries.org/wp-content/uploads/attachments/Policy-brief-39-1997-8073-eng.pdf