The Health Foundation launched an inquiry in October 2020 to gather, analyse and synthesise evidence and insight on the impact of the pandemic, from an extensive range of sources. Yesterday they released their report.
The inquiry set out to answer two key questions:
- How were people’s experiences of the pandemic influenced by their pre-existing health and health inequalities?
- What is the likely impact of actions taken in response to the pandemic on people’s health and health inequalities – now and in the future?
It was not within the scope of the inquiry to formulate policy recommendations but the report did highlight two key areas to create a more resilient society:
- immediate action to address the harm caused by the pandemic and prevent longer term scarring effects;
- building resilience for the longer term.
This extensive review covers 94 pages of analysis that highlights the inequalities that emerged during the pandemic. A selection of key findings follow.
- The single biggest factor influencing differences in COVID-19 mortality between countries was the timing of restrictions.
- Occupation, living conditions and the ability to access financial support affected risk of exposure to COVID-19.
- In the UK certain groups experienced disproportionate levels of exposure and deaths due to the virus
- Once exposed, people’s pre-existing physical and mental health made them more vulnerable to severe outcomes. People with pre-existing conditions, such as diabetes, obesity, cancer, respiratory disease and underlying mental health conditions were at increased risk of death from COVID-19.
Figure 8 displays age-standardised mortality rates for COVID-19 by deprivation decile relative to the least deprived decile by age (England, March 2020 to May 2021)
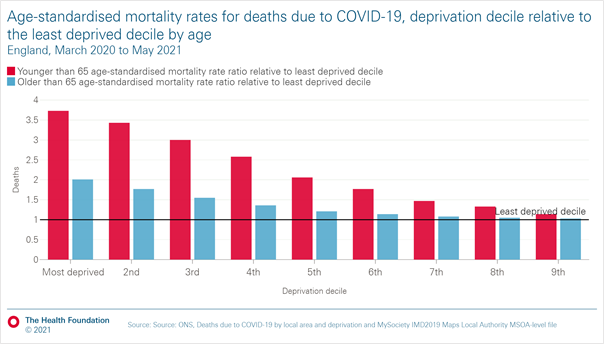
COVID-19 mortality rates were higher among those from more deprived areas than among those from less deprived areas. This differential was higher for those aged under 65
Figure 11 shows excess mortality among care home residents
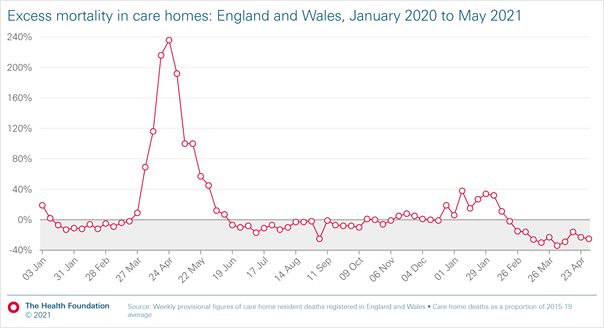
At the peak of the first wave, deaths among care home residents were at more than three times the normal level (excess deaths exceeded 200%).
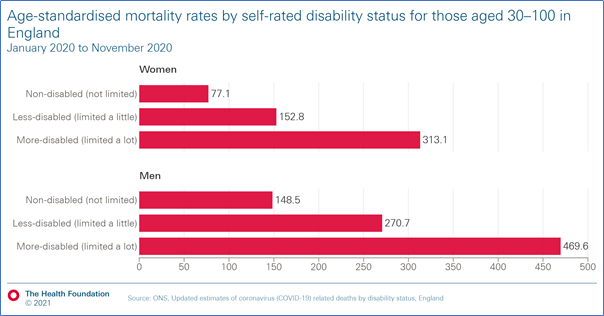
Disability status was also a key factor in outcomes. Disabled people had higher rates of COVID-19 mortality. Women who were disabled had a mortality rate of more than four times that for non disabled women. For men, the rate was more than three times.
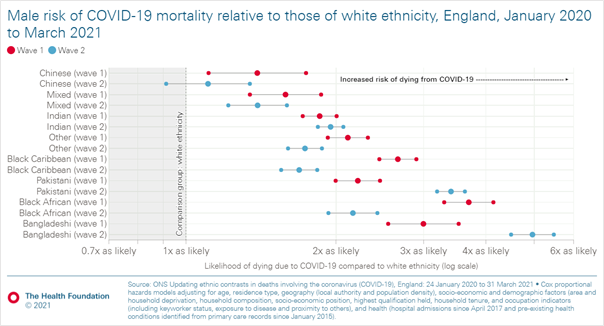
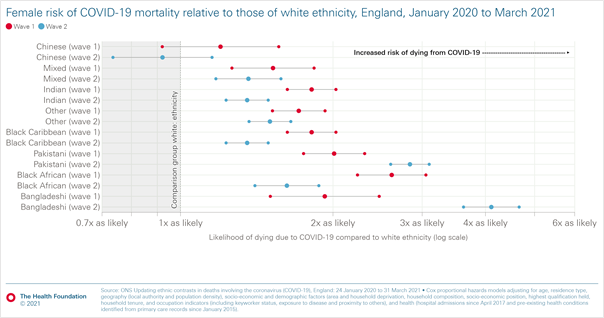
As has been previously highlighted, the risk of COVID-19 mortality in those of white ethnicity was lower than those from ethnic minority communities. Rates for males in figure 14a show that males from ethnic minority communities had an increased risk of COVID-19 mortality in wave one and two.
The risk was higher in the second wave for those from Pakistani and Bangladeshi backgrounds but lower for other ethnic minority communities (after adjusting for other demographic characteristics, socio-economic factors and health conditions).
The next figure displays the same analysis for females.
The pandemic has shown that health and wealth are inextricably linked. A sustainable recovery therefore presents an opportunity to create a healthier and prosperous society, to reduce the stark inequalities exposed by the pandemic.
‘The legacy of the pandemic is all around us in unmet health need, mental health problems, gaps in educational attainment, loss of employment and financial insecurity. If we are to avoid these becoming long-term scars, it’s time to confront our choices about how we value people.’
Dame Clare Moriarty
Chair, COVID-19 impact inquiry Expert Advisory Panel