In this blog, Nicola Oliver reminds us of the principles behind the use of face coverings by the general public and why continued use will help reduce transmission as we look to end other restrictions in England.
The current legal requirement to wear a face covering will no longer be enforced following the planned easing of restrictions on the 19 July. However, Boris Johnson has urged people to take “extreme caution”, including the continued use of face masks in crowded and enclosed spaces.
There is significant evidence that aerosol transmission is a key route for infection with research also suggesting that SARS-CoV-2 remains infectious in aerosols for up to 2 hours.
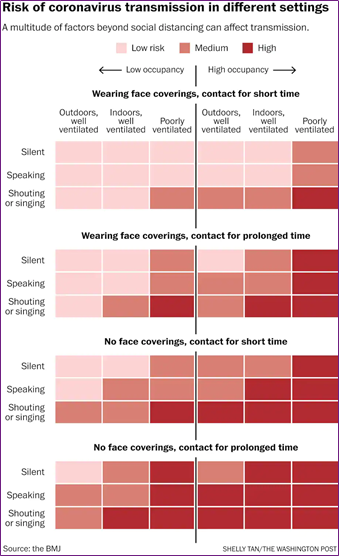
As one might expect, there is a graded risk of aerosol transmission dependent upon multiple factors including physical activity, distance between people, time and the use of a face covering.
In June 2020, we published a bulletin that reviewed the evidence-base at the time for the use of face coverings to reduce the chain of transmission of SARS-CoV-2.
One of the arguments against the use of face masks for personal protection by the public is that there was a lack of evidence. A team led by Professor Trisha Greenhalgh recommends the use of face coverings and point to the precautionary principle, i.e., a strategy for approaching issues of potential harm when extensive scientific knowledge is lacking.
A noted Consensus Statement on the precautionary principle defines the principle: ‘When an activity raises threats of harm to human health or the environment, precautionary measures should be taken even if some cause-and-effect relationships are not fully established scientifically’.
Or to put it simply, it’s better to be safe than sorry.
Recent reviews of the effectiveness of mask-wearing continue to support their use given what we understand about aerosol transmission. In this technical review, the authors provide a useful summary of the selection of materials, mask specifications, relevant laboratory tests, and respiratory virus transmission trials, concluding that face mask wearing prevents COVID-19 infection.
Personal choice regarding the use of newly restored freedoms will likely to shape the future debate on the use of face coverings in public spaces. The use of face coverings is only one of the many non-pharmaceutical interventions that we can use to prevent transmission, but is likely to have the most cost-effective impact given what we know about aerosol transmission.
Greenhalgh et al continue to recommend the use of face coverings, with due consideration of some of the arguments against:
- Masks and face coverings, if widely worn, may substantially reduce the spread of COVID-19.
- The benefits of mask wearing seem to outweigh the harms when COVID-19 is spreading in a population.
- Randomized trials are sparse and have not addressed the question of source control.
- Psychological effects of masks are culturally framed and shape acceptance and adherence.
- Mandated masking involves a tradeoff with personal freedom.
The government recommends the continued use of face masks in crowded areas and on public transport, despite the removal of a legal requirement. As we outlined more than a year ago, most of the evidence points in the same direction: mask wearing reduces person-to-person transmission and could form part of a strategy that reduces the risk of transmission from asymptomatic carriers, potentially also reducing the viral load if there is transmission.