Conflict
The news has brought coverage of the conflict in Ukraine. We are witnessing internal displacement of people, and refugee movement across Europe. Russia and Belarus have had sanctions imposed, which will affect those living there. Consequences are reverberating around the globe. This blog discusses the impact of conflict and the need for public health. The context of course is the COVID-19 pandemic.
Conflict can have large impacts on health, mortality and wellbeing. Similarly, political and economic shocks impact health outcomes. Fragile states, too brittle to absorb shocks, feel these outcomes disproportionately. One shock might be a big increase in the cost of basic food and fuel. Another might be an epidemic of infectious disease for a health system in distress. In due course, we are likely to hear more about such unfortunate consequences.

In a country where conflict is occurring there is an immediate need to treat the wounded and provide food and shelter to those displaced. Infrastructure for clean water, sanitation and health services is vital. The health of internally displaced people is protected by such infrastructure where refuge is found. Unfortunately, infrastructure can be damaged, even targeted. The recent strike on a maternity hospital in Mariupol has highlighted this risk.
Migration
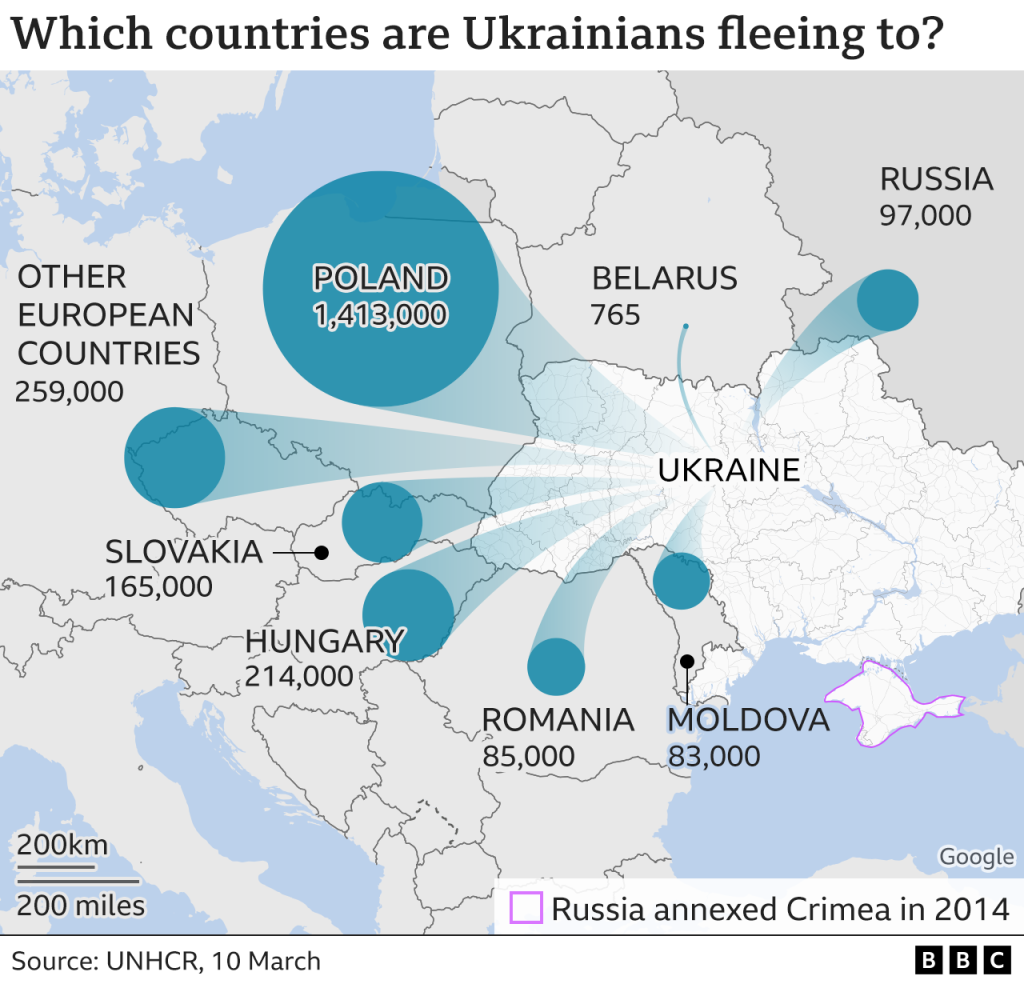
Infrastructure does exist in those countries providing safety to refugees. But two years into the pandemic response health systems are thinly stretched. Public health surveillance, twinned with preventative care for displaced populations, is needed. The sheer numbers makes this challenging. Over two million people are estimated to be on the move.
Where there is mass migration and crowding there is opportunity for infectious disease to spread. For example in evacuation transport, camps, and bomb shelters.
COVID-19 containment is part of the challenge. Only 35% of Ukraine’s population is fully vaccinated. But other infectious diseases are a problem too. Ukraine made efforts to increase vaccination over 2017 to 2019. However, it had over 10 years below recommended levels for HepB3, measles, and DPT. There have been recent outbreaks of highly infectious measles. Vaccination rates for incurable polio are low.
There will be a need to continue treatment for those with diseases such as diabetes and cancer. Health systems will need to cope with these needs, in addition to existing waiting lists.
The images below show the scale of migration within Europe and the COVID vaccination rate for countries welcoming refugees. Vaccine distribution has not been equitable and uptake also varies. Some countries seeing larger migration have vaccine coverage below 70%.
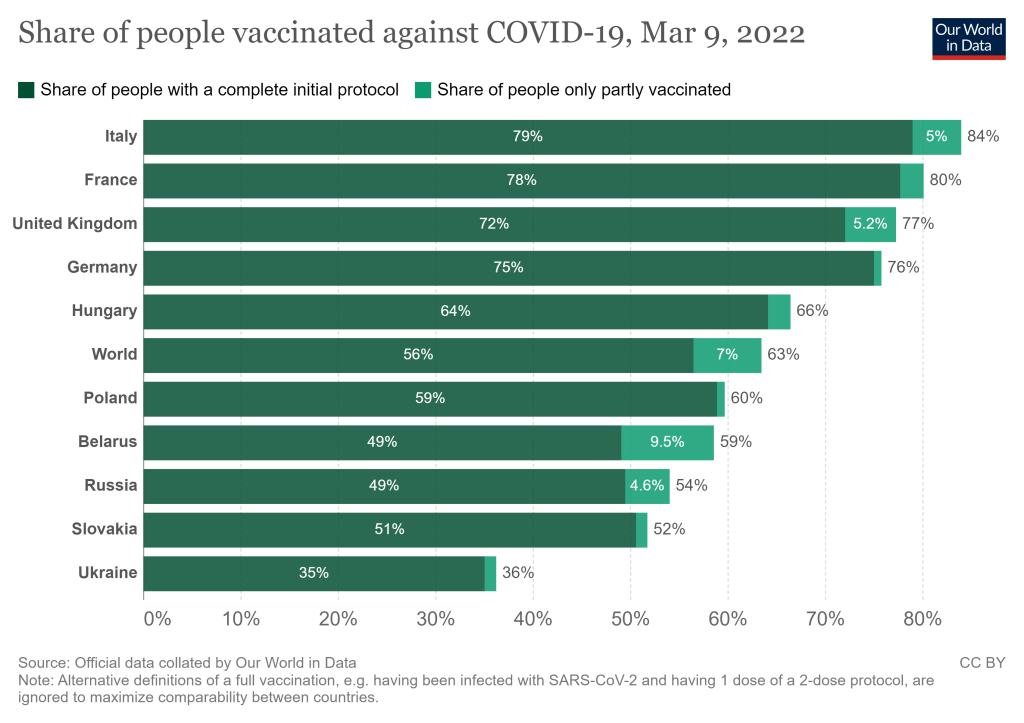
In addition, pandemic disruption to health services has had an impact on routine childhood immunisation within Europe.
Public health authorities must put vaccination programs and surveillance systems in place. This will help to contain and prevent outbreaks of infectious diseases. An epidemic could put more pressure on already thinly spread health systems.
The Longer Term
This blog covers only some short-term impacts of conflict, and the need for public health. There will be wider and longer-term implications. Political and economic shocks will disproportionately affect some populations and states.
Public health response will be vital to protecting life and health for those fleeing conflict. And also to those citizens globally who provide refuge or live with the implications of sanctions.