Summary
There is intrinsic uncertainty in associating a deterioration of health with an illness suffered months earlier. Where the prevalence of an illness is on a global scale, as with COVID-19, then the potential pathological consequences (sequelae) warrant exploration ahead of rigorous multi-year longitudinal studies. The Post-Acute Sequelae of SARS-CoV-2 infection (PASC), commonly known as Long Covid, are a source of increasing public health anxiety, particularly regarding neurological issues. Recent neurological research raises the spectre of non-reversible neuronal injury, even in the absence of severe respiratory disease. As COVID-19 becomes endemic, sickness and disability insurance products could be adjusted to provide appropriate financial support for those whose lives may be upended by Long Covid.
Introduction
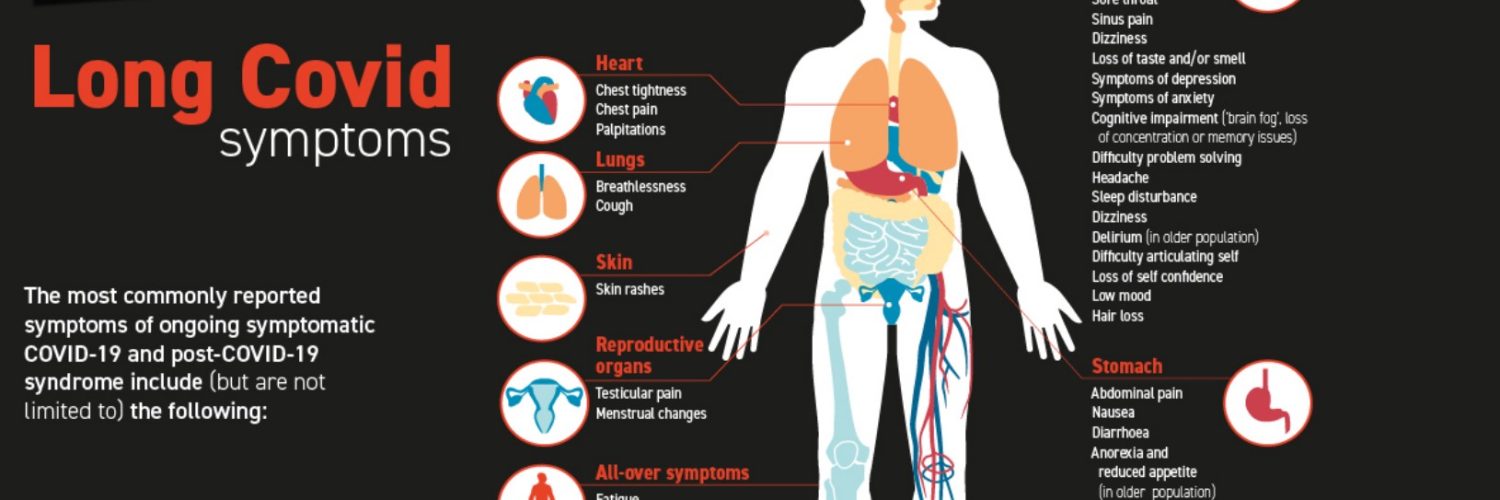
A sizeable proportion of those who have recovered from COVID-19 may experience some lingering symptoms, which may last for months. The most common of these are fatigue, shortness of breath, loss of taste and smell, and cognitive dysfunction. But there are numerous other symptoms including anxiety, depression and muscle aches[1]. These are aggregated as Post-Acute Sequelae of SARS-CoV-2 infection (PASC), more commonly known as Long Covid. Given the time elapsed since an individual’s COVID-19 infection, there is inevitably some uncertainty over the causal connection with any subsequent health deterioration. Diligent longitudinal studies over a number of years will be required to clarify the Long Covid population risk.
In the UK, monthly national self-reporting surveys allow regular updates of Long Covid prevalence, thus providing an observational window into the evolving Long Covid risk. As of May 2022, an estimated 1.8 million people living in private households in the UK (2.8% of the population) self-reported Long Covid symptoms persisting for more than four weeks after the first suspected infection. This is less than 10% of the 22 million UK reported Covid cases; however, the 1.8 million does not include those living in care homes. An international systematic review and meta-analysis of Long Covid prevalence found a wide range of reported prevalence, with much higher prevalence in some populations such as those who had been hospitalised with COVID-19[2]. A community study of more than 600,000 people in England found more than 20% of those testing positive for COVID-19 had at least one persisting symptom after 12 weeks[3].
Data gathering and Survivor Corps
With millions of people afflicted by Long Covid, there is an opportunity for citizen scientists to contribute to mass data gathering, and advance the cause of personalized medicine[4], taking individual variability into account. Early on, patients started sharing their experiences on Twitter, drawing attention to possible COVID-related sequelae. But to make a major societal difference, a more organized data-gathering approach was needed.
Serendipity has always expedited medical advancement; developments addressing one medical issue have often (and fortuitously) turned out to be beneficial elsewhere. On 9 March 2020 Diana Berrent,a 45 year-old New Yorker and former lawyer, was infected with COVID-19. On recovery after spending 18 days in isolation, Diana was eager to help others recover through donating convalescent plasma. She was a good empathetic communicator with a legal background, who, as a Long Covid survivor, could lobby forcefully for change in public policy on the treatment and management of Long Covid, including issues such as financial support and health insurance.
In order to encourage others to follow her example, on 24 March 2020 she set up a Facebook group which she named Survivor Corps. It soon became clear found that many members were not recovering. As the pandemic continued, many Survivor Corps members were struggling with symptoms for weeks or months.
Long Covid is the first patient-identified illness rooted in a social media network. With more than 200,000 members, Survivor Corps is a vital aggregate source of information about Long Covid. The voluntary collective public sharing of personal health information about newly emergent illnesses can generate new data and fresh insights for the medical research community. If a patient presents with some unfamiliar Long Covid symptom, this is confidential information, not to be shared outside a doctor’s surgery. Yet, Survivor Corps members have self-reported extreme neuropathic pain, Parkinsonian tremors, COVID-onset diabetes and lupus, adrenal fatigue, hearing and vision loss, as well as dental problems due to vascular jaw damage.
Diana Berrent has disclosed that many members’ lives have been so blighted by Long Covid that they have ended them, and has warned of a tsunami of Long Covid suicides. There may be direct neuropsychiatric effects of COVID-19 that may increase the risk of suicide. There is no way of gauging the number of suicides due to an intolerable burden of Long Covid. If a young athlete took his or her own life after being crippled by Long Covid, it would be registered simply as suicide. As of October 2021, a new Post-Covid international disease classification code (ICD) has been introduced as a critical step to improve patient care, as well as for tracking and research purposes. It is already known that older patients aged 65 or more with severe COVID-19 have an increased 12-month mortality risk[5].
As with all social media content, the reliability and authenticity of information contributed by some Survivor Corps members may be open to query. But as an influential patients’ advocacy group, Survivor Corps serves a practical societal function in galvanizing and expanding scientific research on Long Covid. Given the experiences of Survivor Corps members, Diana Berrent believes that we will look back on it largely as a neurological disease. Time will tell, but there is a growing body of scientific evidence that COVID-19 is a severe multi-system inflammatory disease disorder with potentially devastating long-term neurological features rather than just a severe respiratory infection[6].
Neurological issues
Even mild cases of COVID-19 may lead to a loss of cognitive function and a reduction in brain volume equivalent to at least one year of normal ageing. This is a recent finding from brain scans taken both before and, on average, 4.5 months after coronavirus infection[7]. A key open question is whether this brain tissue damage resolves in the longer term.
Individuals who have recovered from COVID-19 perform worse on a range of cognitive tests than would be expected given their age and demographic profiles. For those who had ventilator treatment, the score reduction was worse than ten years of decline[8]. Severe COVID-19 illness is associated with significant objectively measurable cognitive deficits that persist into the chronic phase.
Neuropsychological testing amongst the elderly has further shown that COVID-19 is capable of eliciting persistent measurable neurocognitive alterations, particularly in the areas of attention and working memory[9]. These effects, which degrade basic social and living skills, may represent an early stage of cognitive impairment in the elderly, and so may lead to an increased prevalence of dementia amongst the elderly. A further concern in future is the prospect of increased dementia amongst the middle-aged afflicted with Long Covid in their thirties and forties. Amongst other economic and social disruption, this would affect sickness and disability insurance coverages.
Serena Spudich, a professor at the Yale neuro-COVID clinic, considers the most likely cause of the cognitive dysfunction known as brain fog to be inflammation created by immune response[10]. Neurological complications are often among the first symptoms of SARS-CoV-2 infection and can be the most severe and persistent. They can also affect people of all ages, and with varying degrees of disease severity.
In order to improve understanding of the neuropathogenesis, a study of brain pathology has recently been undertaken in non-human primates[11]. The development of animal models is critical for progressing this understanding rapidly. Neuroinflammation has been found in non-human primates with SARS-CoV-2 infection. Pathological investigation found severe brain inflammation and injury consistent with reduced blood flow or oxygen to the brain, including neuron damage and death. This research provides important insight into the mechanisms underlying central nervous system disease, observed even in the absence of severe respiratory disease. It may suggest that hypoxic brain injury, when the brain does not get enough oxygen, is a common complication of COVID-19.
Neuronal degeneration may indicate that non-reversible neuronal injury could be significant for those suffering from Long Covid. This would suggest the need for long-term neurological follow-up of persistently symptomatic convalescent patients and underlines the importance of establishing benchmarks for Long Covid prevalence. Observations of neuroinflammation and neuronal injury in acute COVID-19 cases may accelerate or trigger future development of neurodegenerative diseases such as Alzheimer’s Disease.
As a mitigation of the Long Covid risk, patients who are infected after full vaccination are 50% less likely to develop Long Covid, according to a UK Health Security Agency review of evidence from 15 UK and international studies[12]. The Long Covid risk of patients vaccinated after infection is also a cause of public health anxiety. In a community-based study of adults aged 18 to 69 years infected with SARS-CoV-2 before vaccination against COVID-19[13], it was found that the odds of experiencing Long Covid symptoms that persisted for at least 12 weeks decreased by an average of 13% after a first COVID-19 vaccine dose. Receiving a second vaccine dose was associated with a further 9% decrease in the odds of Long Covid, and statistical evidence suggested a sustained improvement after this, at least over the median follow-up of 67 days.
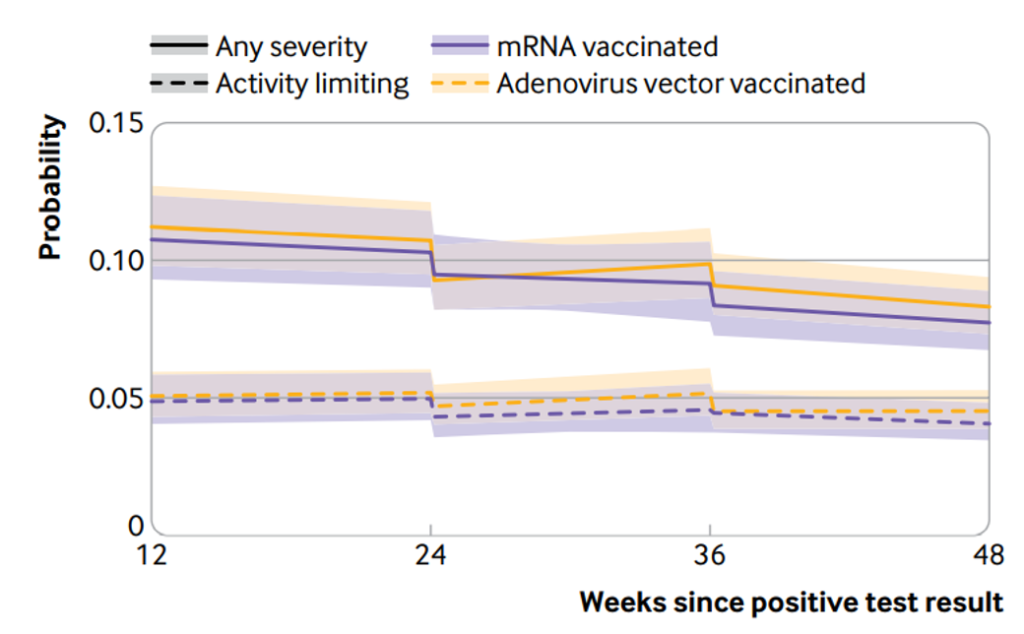
Vaccine type may not matter. As shown in the figure below taken from that study, no statistical evidence was found of heterogeneity in the association between vaccination and Long Covid symptoms according to Adenovirus or mRNA vaccine type. The figure shows modelled probabilities of Long Covid for a hypothetical study participant who received a first dose of an adenovirus vector or mRNA vaccine 24 weeks after SARS -CoV-2 infection and a second dose 12 weeks later. Probabilities are shown for participants of mean age (50 years) and in the modal group for other covariates.
Final thoughts
As COVID-19 becomes endemic, new public health protocols should be established for Long Covid. For the working population, sickness and disability insurance products could be adjusted to provide appropriate financial support for those whose lives may be upended by Long Covid. This is a potentially valuable societal contribution from the insurance industry to mitigate the need for a Long Covid suicide help-line, which has been advocated by Diana Berrent[14].
[1] ONS (2022) Statistical Bulletin, 6 May.
[2] Chen C. et al. (2022) J. Infectious Diseases, 16 April.
[3] Whitaker M. et al. (2022) Nature Comms, 12 April.
[4] Petersen C et al.. (2019) JAMIA, 3 December.
[5] Mainous A.G. (2021) Frontiers in Medicine, 1 December.
[6] Norouzi M. (2021) Molecular Neurobiology 25 March.
[7] Douaud G. et al. (2022) Nature, 7 March.
[8] Hampshire A.(2021) eClinical Medicine, May.
[9] Lauria A. (2022) Clinics in geriatric medicine, 8 May.
[10] Blackmann I. (2022) Yale medicine news. 26 April.
[11] Rutkai I. (2022) Nature Comm., 1 April.
[12] Mahase (2022) BMJ, 16 February.
[13] Ayoubkhani D. et al.(2022) BMJ. 18 May.
[14] Berrent D. (2022) New York State Long Covid Symposium, 3 February.